In this post
Lorem ipsum dolor sit amet
Lorem ipsum dolor sit amet
HRA, FSA, HSA, LSA, QSA (okay, we made that last one up!). The acronym land of benefits can be overwhelming. This post is going to focus on HRAs, or health reimbursement arrangements. They are often confused with an HSA (health savings account). While there are some tax-advantaged similarities between the two, there are a few key differences.
What is an HRA?
An HRA is an employer-funded account that offers employees money to pay for eligible healthcare expenses.
There are two key types of HRAs: group coverage HRAs and expected benefit HRAs. Group coverage HRAs are offered in conjunction with the employer’s group medical plan to reimburse employees for out-of-pocket medical expenses that are not fully covered. There is no limit on employer contributions, and they are only available to employees who are enrolled in the employer’s group medical plan, which cannot be a high-deductible health plan.
Excepted benefit HRAs are similar to the group coverage HRA with the key benefit being medical care that is not covered or not covered fully by the group medical plan. However, they are available to all employees, regardless of enrollment in the employer’s group medical plan. There is also a maximum employer contribution of $1,800 per year.
What's the difference between an HRA and HSA?
There are a few important HRA and HSA differences to be aware of. HRAs are owned by the employer, which means that if an employee were to leave the organization, unspent funds stay with the employer. HSAs are owned by the employee (although employers can contribute), so employees keep unused funds if they leave the organization.
HRAs are often paired with a high-deductible health plan (HDHP). But under a new law passed in 2016, small businesses with fewer than 50 employees may be eligible to offer an HRA without an associated health insurance plan. Final regulations now allow employers of any size that don’t offer a group health plan to fund a premium-only HRA that employees can use to buy individual coverage.
Additionally, as part of the Coronavirus Aid, Response and Economic Security (CARES) Act signed into law in March 2020, HRA funds — along with those from HSA and FSA funds — can now be used to pay for any over-the-counter medications without a prescription.
Can I offer both an HRA and HSA?
Yes, both may be offered. However, there are certain requirements for both to be used compliantly. To be eligible for an HSA, employees must be covered under a qualified HDHP. Any other policies offered to employees must be HSA-qualified, including an HRA. There are several types of HRA plans that are compatible with HSAs:
- Limited-purpose HRA: This arrangement only reimburses employees for HRA eligible expenses that do not count toward the HDHP deductible, including dental, vision, and preventive care like checkups, mammograms, smoking cessation, and weight loss.
- Suspended HRA: Before the HRA coverage period begins, an employee can choose to suspend it and forgo reimbursements during the suspension period, allowing them to remain HSA-eligible. Similar to the limited-purpose HRA, employees can still receive reimbursements for expenses that are exempt from the HDHP deductible, like dental, vision, and preventive care.
- Post-deductible HRA: This type of HRA essentially has its own deductible. Employees can receive reimbursements for qualified medical expenses, but only after they’ve met the minimum allowable HDHP deductible. For 2022, the minimum deductible is $1,400 for individual HDHP coverage and $2,800 for family HDHP coverage. For 2023, it will increase to $1,500 for individual and $3,000 for family.
- Retirement HRA: With a retirement HRA, employees are only reimbursed for medical expenses incurred after they retire. They can use their HSA up until retirement, at which point they are no longer eligible to make contributions to an HSA. After that, they can begin to use their HRA funds.
HRA can only reimburse employees for expenses exempt from the HSA deductible requirement. They include items like health insurance premiums, dental and vision premiums, and insurance-covered wellness exams like mammograms.
Questions to guide you
When designing your HRA, you will need to ask yourself and decide:
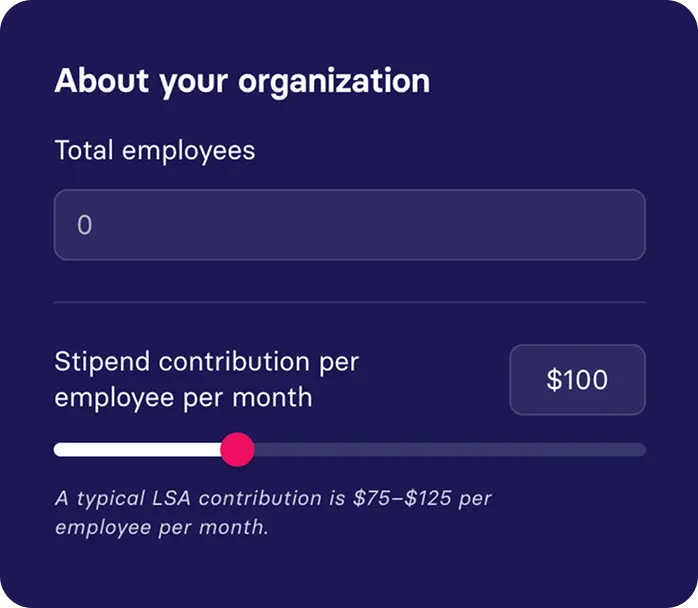
- How much should we fund the HRA?
- Who pays the deductible first - employees or the employer?
- Can unused funds be rolled over to the following year?
- Which expenses can be covered by the HRA?
Benefits of an HRA
HRAs are funded by the employer, which allows them the flexibility to tailor the funds to their employee population’s unique needs. These can take the form of specialty HRAs that allow employers to support medical needs that might not fall under their health insurance plans, such as fertility treatments, gender confirmation surgery, or medical travel to access out-of-state care. Many employers choose not to include these types of benefits in group health insurance because they can drive up premiums for the entire group. With an HRA, employers avoid absorbing these costs into their health plan while still providing a way for employees to pay for expensive medical care without dipping into their own pockets. Additionally, HRA accounts do not need to be pre-funded, so employers have a unique opportunity to control cash flow.
Similar to an HSA, spending on eligible medical expenses are tax-deductible for employers and employees alike. Employees can even use the HRA to pay a portion of their insurance premiums, which allows employees to select the best plan based on their location, health needs, and family.
Getting started
HRAs allow your organization the unique opportunity to control costs while still offering significant healthcare benefits to their employees. Building your HRA will depend on many factors including your company size, current health insurance plan, employee population, and many more. Planning for your HRA and developing a plan for the distribution of the funds and reimbursement is complex. Have questions about what it takes to craft an HRA program and offer employees an easy-to-use Visa card? Reach out at sales@getbenepass.com.