In this post
Lorem ipsum dolor sit amet
Lorem ipsum dolor sit amet
Offering health benefits is about striking the perfect balance between affordability and value. You don’t want to invest in an expensive plan that doesn’t fulfill your employees’ needs, nor do you want your workers to shoulder too much of the cost.
Integrated health reimbursement arrangements can be an effective solution, but are they the best fit for your business? Our guide explains the advantages of offering integrated HRAs, how they differ from alternatives, and how to implement your healthcare benefits using Benepass.
What is a health reimbursement arrangement (HRA)?
A health reimbursement arrangement is a type of employer-funded medical benefit. Four different types are available: integrated or group coverage HRAs, individual HRAs, qualified small employer HRAs, and excepted benefit HRAs. Note: not every employer has access to every type of HRA.
An integrated or group coverage HRA requires enrollment in a complementary group health plan and is designed to cover eligible medical expenses, such as mental health support or fertility assistance, unavailable within your existing plan. Some employees will also use their HRA to offset the cost of their deductible, making it more affordable to access the healthcare they need.
HRAs vs. HSAs
Don’t be confused by the similarity of these acronyms—HRAs and HSAs serve different purposes, although they’re both available as pre-tax benefits.
- Health reimbursement arrangements (HRAs) are an employer-funded benefit. Employees are reimbursed for HRA eligible expenses incurred according to the terms of the HRA plan.
- Health savings accounts (HSAs) are funded by both employers and employees enrolled in high-deductible health plans. A health savings account is typically portable, meaning the funds remain with the employee even after changing jobs.
Why offer an integrated HRA to your employees?
There are several ways to support your employees’ healthcare needs. So, what advantages does an integrated HRA offer over alternative medical benefits?
Improved inclusivity
Inclusive benefits ensure all employees in your organization have access to the benefits you offer and the investment you make in them. For example, if you invest in an HDHP with fantastic coverage for medical-related travel that some of your workers will never need, that’s not the most inclusive benefits strategy.
Instead, integrated HRAs offer a customized approach, allowing employees to supplement their group health plan if they need access to a wider variety of medical expenses, such as gender confirmation surgery, OTC prescriptions, or emergency treatments. An HRA allows you to be inclusive by offering a broader benefits selection.
Lowered costs
The best part about offering this wider range of benefits is that it doesn’t drive up the total cost of your group health plan. Instead of paying for expanded benefits for your entire workforce, the employer only pays for what individual employees need. As a reimbursement model, employers pay for the expenses incurred rather than investing upfront in a one-size-fits-all package.
Healthy employees
According to the Policygenius Health Insurance Survey, 28% of people with medical coverage can’t afford to pay the deductible. Worse, a staggering 45% of insured Americans have avoided seeking medical support because they knew or feared their insurance wouldn’t fully cover the costs. Access to health reimbursement arrangements leads to better outcomes for your employees by ensuring everyone can afford necessary care without the financial strain of paying for expensive deductibles.
Tax benefits
Contributions to an HRA offer tax advantages for both employers and employees. The Internal Revenue Service permits employers to deduct contributions to their employees’ HRA plans as a business expense. The reimbursements are also tax-free for employees, making it a valuable addition to any employee’s benefits package.
How a group coverage HRA works
Group coverage HRAs differ from alternatives such as individual coverage HRAs or qualified small employer HRAs. Here’s how they work:
- Employees must be enrolled in a group health insurance plan approved by the Affordable Care Act. This ensures the HRA complies with ACA mandates, including coverage standards and preventive care benefits.
- Employers can contribute whatever they like to their employees’ HRA—there are no maximum or minimum limits.
- Any unspent funds may be rolled over to the following month or year, depending on the platform and the terms of your plan. Alternatively, the employer will receive the money back.
- Employers list eligible expenses such as copays, deductibles, or other costs.
- Employees submit receipts for these expenses to the employer, who reimburses them from the HRA funds.
Alternatives to integrated HRAs
If integrated HRAs aren’t a good fit for your organization, the following alternatives are available:
Individual Coverage HRAs
Individual coverage HRAs reimburse employees for individual health insurance coverage they purchase on their own. They can be combined with other medical benefits, such as an HDHP or FSA.
Qualified Small Employer HRAs (QSEHRAs)
Qualified small employer HRAs (QSEHRAs) are designed for businesses with fewer than 50 full-time employees. They work similarly to group coverage HRAs, but there are limits on how much employers can contribute annually. According to the “Employer’s Guide to Fringe Benefits,” the current limit for HRAs is $6,150 per individual and $12,450 per family.
Excepted Benefit HRAs
Excepted benefit HRAs (EBHRAs) were introduced in January 2020 and are designed to cover limited benefits, such as dental and vision expenses, not covered by a primary group plan. EBHRAs differ from integrated HRAs because they have a maximum contribution limit of $2,100 for 2024. However, there’s no requirement for group health plan enrollment.
How to set up an integrated HRA
The instructions below are how most HRA vendors will offer their health reimbursement arrangements. (Hint: we make it even easier at Benepass.)
1. Set up your group coverage HRA
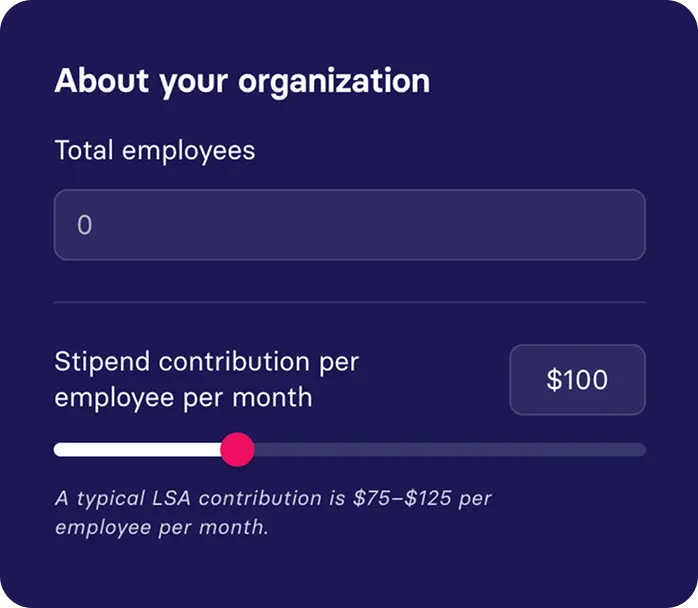
Begin by deciding how much pre-tax money you’ll offer employees each month based on your overall employee benefits strategy and budget.
2. Provide a list of eligible medical expenses
Determine what the HRA is designed to cover and communicate this to your employees so they fully understand what is available. Check IRS Publication 502 for an extensive list of eligible expenses, including who can receive them, for example, spouses and dependents.
3. Employees make medical purchases
Employees can spend their HRA allowance as needed. For example, they may pay upfront for personal therapy sessions if listed as an eligible expense.
4. Employees request reimbursement
Employees must provide detailed records, including:
- Name and cost of the medical item or service
- Date of purchase
- Name of the vendor
- Receipts
They submit this evidence to their HR or benefits team to process the reimbursement admin for the HRA.
5. Employers pay the expenses
Your team will review and approve (or reject) the reimbursement and pay the money back to their employee. Payment options include:
- Non-taxable line item added to paycheck
- Cash or check
- Direct deposits or bank transfers
Offer superior integrated HRAs with Benepass
The problem with the traditional reimbursement approach is that employees must first pay out of pocket before receiving their expenses back. With 65% of Americans currently living paycheck to paycheck, this method simply isn’t feasible for most people. The risk is that employees will skip seeking medical support when they need it.
Benepass offers a better way. Using our card-first technology, employees can charge their medical expenses directly to their Benepass card, so there’s never a gap between seeking medical care and having the funds to pay for it. It’s an equitable approach that ensures all employees can access the support they need, regardless of their salary or financial status.
Ready to see our benefits platform in action? Book a free Benepass demo today or contact sales@getbenepass.com to connect with a benefits specialist.