In this post
Lorem ipsum dolor sit amet
Lorem ipsum dolor sit amet
Shiny, attractive benefits enhance your employees’ personal and professional lives and cement their loyalty to you as an employer. But behind every comprehensive benefits package is a huge amount of red tape.
Employers must comply with numerous laws and regulations related to benefits and perks. It’s daunting, but it’s important—and failure to comply can result in serious consequences. This guide will help you navigate the complexities of employee benefits compliance so that you can focus on what really matters: keeping your employees happy and engaged.
What is employee benefits compliance?
Employee benefits compliance ensures that a company’s benefit plans and practices satisfy applicable federal, state, and local laws and regulations. Non-compliance can result in legal consequences and penalties for the employer, loss of reputation, and a negative impact on employee morale.
8 types of employee benefits compliance to be aware of
Employee benefits compliance involves being well-versed in a variety of regulatory areas. Here are the eight types of compliance you need to be particularly vigilant about and incorporate into your benefits administration strategy:
Affordable Care Act (ACA)
The Affordable Care Act is a federal law that requires certain employers to provide affordable health insurance coverage to their employees.
Organizations with 50 or more full-time employees are subject to the ACA’s shared responsibility provisions, also known as the employer mandate. They must offer minimum essential coverage that meets affordability and minimum value requirements to at least 95% of their full-time employees and their dependents.
To comply with the ACA, employers should regularly review and update their health insurance offerings to ensure they meet the relevant requirements, including reporting requirements. They should also accurately track employee hours to determine if they fall under the full-time equivalent threshold and are subject to the employer mandate.
Relevant forms include:
Consolidated Omnibus Budget Reconciliation Act (COBRA)
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is also known as Continuation of Health Coverage. This federal law requires employers with 20+ employees in the prior year to offer a temporary health insurance continuation of their group health plan to employees and their covered dependents. This kicks in when they lose their job voluntarily or involuntarily, reduce working hours, or experience other qualifying events such as death or divorce.
Employers must provide COBRA notices to eligible individuals within specific timeframes and allow them to continue their health insurance coverage for up to 18 months (or up to 29 months for certain disability extensions) by paying the total premium cost of up to 102%. Relevant notices include:
- General notice: Provided within the first 90 days of coverage, it explains COBRA rights and basics to covered employees and their spouses.
- Election notice: Issued within 14 days of a qualifying event, it details the right to choose COBRA continuation coverage, including information on coverage options, duration, costs, and how to elect coverage.
- Notice of unavailability: Explains why an individual is not eligible for COBRA coverage after a qualifying event.
- Notice of early termination: Informs about the early end of COBRA coverage, including the reason and termination date.
To comply with COBRA, employers should educate themselves on the notice requirements and establish processes for notifying eligible employees. They should also keep accurate records of employees’ qualifying events and offer them continued coverage at the correct premium rates.
Health Insurance Portability and Accountability Act (HIPAA)
The Health Insurance Portability and Accountability Act protects the privacy and security of individuals’ health information. Employers that provide self-insured group health coverage must comply with HIPAA’s Privacy, Security, and Breach Notification rules as a federal law.
Organizations with group health plans should have policies and procedures for patient protections to ensure confidentiality when handling employee medical records and protected health information. They should also conduct regular risk assessments, train relevant employees on HIPAA compliance, and implement safeguards against data breaches.
Employee Retirement Income Security Act (ERISA)
The Employee Retirement Income Security Act (ERISA) sets the standards for private industry employers offering their employees retirement, pension, or welfare benefit plans.
As a federal law established in 1974, ERISA compliance requires employers to provide employees with specific information about their benefit plans, such as plan documents and summary plan descriptions. It also establishes fiduciary responsibilities for those managing the plan’s assets and prohibits certain discriminatory practices.
To comply with ERISA, employers should ensure they have the necessary documents and disclosures in place. They should also understand their fiduciary duties and act solely in the best interests of plan participants.
Relevant forms include:
- Form 5500 which must be filed electronically using EFAST2-approved third-party software or IFILE
Medicare
Medicare is a federal health insurance program for individuals aged 65 and older, certain younger people with disabilities, and those with End-Stage Renal Disease (ESRD) and Lou Gehrig’s Disease (ALS). Employers must comply with Medicare Secondary Payer rules when providing health insurance to employees who are eligible for Medicare.
To comply, employers should determine if their group health insurance is primary or secondary to Medicare coverage and follow specific guidelines for coordinating benefits. They should also educate employees on Medicare enrollment and their options for coverage. Payroll staff are instrumental to Medicare compliance, as employers are required to withhold Medicare taxes from employees’ wages. Employees contribute 1.45% of their pay, and employers match the contribution for a total of 2.9%.
Relevant forms include:
Health Savings Accounts (HSA)
A Health Savings Account (HSA) is a type of tax-advantaged account that individuals can use to pay for qualified medical expenses. HSAs are usually offered in conjunction with a high-deductible health plan (HDHP) and offer triple tax benefits: Contributions, earnings, and withdrawals are all tax-free.
The IRS sets out minimum and maximum annual deductible costs for HDHPs for 2024:
- Minimum annual deductible = $1,600 for self-only coverage and $3,200 for family coverage
- Maximum annual deductible and other out-of-pocket expenses = $8,050 for self-only coverage and $16,100 for family coverage.
To comply with HSA regulations, employers must ensure their plans meet high-deductible health plans and HSA eligibility requirements. They should also educate employees on the benefits of HSAs and assist them in setting up and managing their accounts.
Relevant forms include:
Flexible Spending Accounts (FSA)
A Flexible Spending Account (FSA) is a tax-advantaged account that allows employees to set aside pre-tax dollars for out-of-pocket healthcare expenses, dependent care, or qualified commuting costs. Employers can offer three types of FSAs as part of their benefits package and must follow specific rules to ensure compliance with the IRS.
- Health Care FSA (HCFSA)
- Limited Expense Health Care FSA (LEX HCFSA)
- Dependent Care FSA (DCFSA)
To comply, employers should establish plan documents outlining FSA eligibility, contribution limits, and qualified expenses. They should also conduct regular nondiscrimination tests to avoid discriminating in favor of highly compensated or key employees. Additionally, employers must properly monitor employee contributions and ensure they don’t exceed the maximum allowed amount.
Relevant forms include:
- IRS Form W-2 (see box 10)
Family and Medical Leave Act
The Family and Medical Leave Act (FMLA) is a federal law that requires certain employers with 50+ employees to provide eligible workers up to 12 weeks of unpaid, job-protected leave for specific family and medical reasons. These reasons include the birth or adoption of a child, caring for a family member with a serious health condition, or an employee’s own serious health condition.
To comply with FMLA, employers should determine if they are covered under the law and establish policies for employee leave. Employers must reinstate employees to their same or equivalent position upon return from leave and continue paying health benefits in their absence. Employers should also educate employees on their rights under FMLA.
Relevant forms include:
- WH-381: Notice of Eligibility and Rights & Responsibilities
- WH-382: Designation Notice
- WH-380-E: Certification of Health Care Provider for Employee’s Serious Health Condition
- WH-380-F: Certification of Health Care Provider for Family Member’s Serious Health Condition
- WH-384: Certification of Qualifying Exigency For Military Family Leave
- WH-385: Certification for Serious Injury or Illness of Current Service Member—for Military Family Leave
- WH-385-V: Certification for Serious Injury or Illness of a Veteran for Military Caregiver Leave
Enforce compliance requirements with Benepass
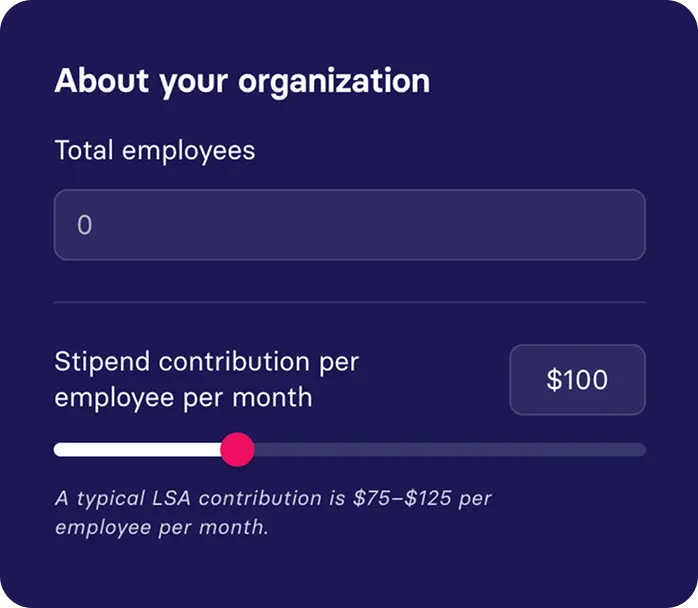
Benepass is a fully compliant benefits administration platform designed to offer incredible employee benefits while keeping companies on the right side of Uncle Sam. Along with delivering a full range of pre-tax benefits (including HSAs, FSAs, Commuter Benefits, and Health Reimbursement Arrangements) and perks programs (including wellness, food, professional development, family benefits, LSAs, remote work accounts, and rewards and recognition programs), Benepass also offers the following compliance features:
- Compliant pre-tax benefits admin, including full plan documentation and summary plan description
- Nondiscrimination testing & 5500s
- Templated employee education materials enabling you to proactively communicate relevant rules to employees
- An employee experience team to support your HR teams
- Automated reporting using integrations with your payroll and HRIS systems to report imputed income for taxable benefits
Ready to ensure watertight employee benefits compliance in your organization? Book a free Benepass demo today or contact sales@getbenepass.com for more information.




.jpg)